Navicular Bone
Accessory navicular bone / external tibial bone
Accessory navicular bone is the presence of an extra bone growth core on the inner side of the navicular bone of the foot where the tibialis posterior tendon is attached.
The main common symptom of patients with this condition is swelling, pain and tenderness, often combined with a flatfoot deformity. Very often pain starts after lng walking periods or impact sports activities like running, jumping and competitive ball games with frequent changes of running direction.
This condition belongs to the congenital conditions as it is present from birth even that it can not be seen in early x-rays due to the cartilaginous nature of immature bones.
The treatment is usually conservative with orthotics and treatment of additional deformities. In case of chronic pain an individual small surgical treatment with removal of the accessory bone can be done, related to the individual findings, with short rehabilitation and very good success rate.
Hip Dysplasia
Hip Dysplasia – HIP Screening
What is a hip dysplasia – DDH
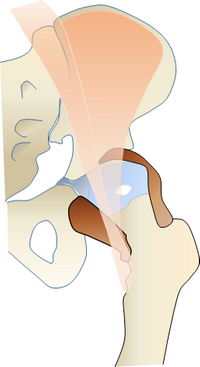
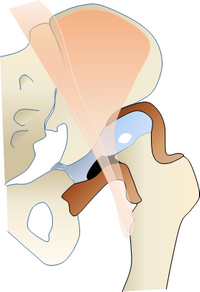
Hip dysplasia is one of the most common pediatric orthopaedic conditions affecting children from newborn age, during childhood with effect even during adulthood and old age. Hip dysplasia is a delay of development of the hip joint. The pelvic part of the hip joint is too small, to steep or not developed anatomically correct. As a result the cavity of the hip joint does not or only minor stabilize the upper part of the femur bone and its articulating part of the femoral head. There are multiple degrees of delay of hip development known, from mild dysplasia to complete dislocation, unilateral or with both the hip joints involved.
Is there a difference in hip dysplasia and hip dislocation?
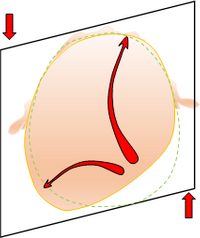
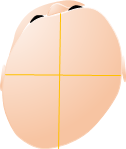
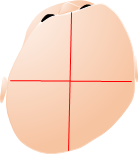
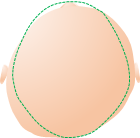
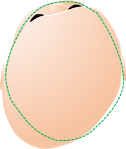
A dysplastic hip can be either centered (a) or displaced/ dislocated (b). In a centered hip the upper part of the femur with its femoral head is still centered somehow within the hip joint fossa acetabuli. In case of a hip dislocation the femoral head has already slipped out of the acetabulum. As a consequence there is an independent development in between these two normally perfectly fitting joint parts with resulting incongruity. A dislocated hip is not able to properly stabilize the joint while walking, hip imbalance with limp will develop.
(a)
(b)
What is the reason for a child developing hip dysplasia?
The exact cause for the development of DDH is still not exactly known. However it is widely believed that hip dysplasia is developmental. This is because hip dysplasia is known to develop around the time of birth, after birth, or even during childhood. Therefore is also why hip dysplasia is often defined as “developmental dysplasia of the hip” (DDH).
Are there risk factors for a hip dysplasia?
General risk factors are for example twin pregnancies, oligohydramnion (low intrauterine amniotic fluid level), breech position, female gender, firstborn and a family history of DDH (Developmental Dysplasia of the Hip). In these cases the incidence of developing a DDH is significantly higher. Specific positioning of babies such as swaddling after birth is known to have negative effect to the hip development.
What are the symptoms of a hip dysplasia in a newborn?
Clinical symptoms which can be seen in newborn are a limitation of abduction possibility of the affected hip joint or leg. Sometimes a fold asymmetry in the upper leg, at the gluteal fold or the labial fold can be seen, especially if one hip is instable and has the tendency to dislocate, then also a leg length discrepancy might occur. The experienced examiner might find signs of hip instability (Ortholani, Barlow) during the examination. Older children might develop gait asymmetries or a limp, rotation anomalies of the legs or tiptoe walking. Mild to moderate hip dysplasia very often cannot be identified by normal clinical examination alone. This needs further on examination. Therefore the golden standard of diagnosis is meanwhile the ultrasound examination within the first months of life of a newborn.
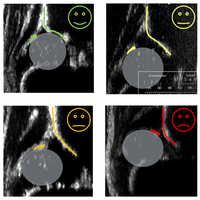
It is generally recommended to have at least one valid picture of the hip to visualize and measure the hip anatomy. This can be done easily and without the need for radiation with ultrasound in a newborn.
What is hip Screening with Ultrasound
Ultrasound is the golden standard of examination to evaluate if a child is affected by a hip dysplasia. Ultrasound is pain free and does not contain any kind of radiation. Pregnant woman know ultrasound as a pain free possibility to see their children and its heartbeat already in the uterus even before the baby is born. This ultrasound technique allows as soon as the child is born to see the developmental status of the hip joints. The ultrasound examination can be done from the date of birth until the osseous growth centre of the femoral head has developed and hinders the ultrasound beam to approach the deep fossa of the hip joint. This usually happens at the age of about 5 to 6 months in healthy mature babies.
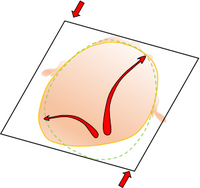
Ultrasound Stages of DDH from healthy hip to displacement
Can any examiner do a hip ultrasound screening?
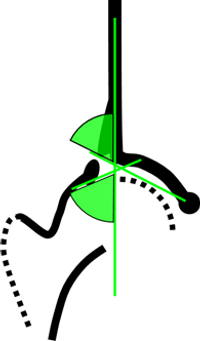
The ultrasound hip screening can be done by a special trained pediatric doctor or pediatric orthopaedic doctor. The standard Ultrasound method for DDH (Developmental Dysplasia of the Hip) is the Graf Method. With this method a hip dysplasia can be diagnosed reliable. Usually a special positioning mattress is used to be sure that standardized examination circumstances are given. A specific ultrasound device with angulation measurement and linear ultrasound probe will allow correct measurement of the hip anatomy.
What is the Graf Method of Ultrasound?
Reinhard Graf is an Austrian Pediatric orthopaedic surgeon, he has been Head of the Stolzalpe Hospital/Austria from 1988 to 2011. Here he developed the Ultrasound hip examination already in the 1970s in Austria. As a general hip screening method to diagnose hip problems it has been established in Austria in 1992 as a mandatory hip screening for newborn. Germany followed in 1996, Switzerland in 1997. Since the screening is established the problem of hip dysplasia in these populations is almost completely disappeared, as treated early, the prognosis is excellent. Since the screening has been established the amount of hip surgeries in these countries is reduced approximately by 50%.
Are there any other methods of diagnosing a hip dysplasia?
In older children where the bone growth development is already more developed the standard examination for hip dysplasia is the x-ray. This will usually be done with special x-ray filters for children and gonad protection to reduce radiation to a minimum.
What happens if your child is diagnosed with hip dysplasia?
If your child has a hip dysplasia, treatment options will be discussed with the pediatric orthopaedic surgeon. The treatment depends on the age of the child and severity of the dysplasia. In a vast majority of the cases conservative therapy can be done if the diagnosis is confirmed early. Then certain splints and braces will be worn by the baby for a period of time until the hip development has become physiologic. Usually these splints and braces are applied in a certain hip flexion abduction position which allows the hip to develop regular.
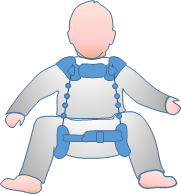
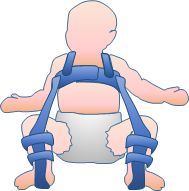
What kind of splints or braces are usually used for hip dysplasia treatment?
Depending on the age of the child and severity of the dysplasia different splints are taken. Commonly used splints are:
Tűbinger splint
Pavlik Harness
Rhino cruiser
How do I know how to apply the splint or brace?
The treating doctor will explain detailed about the splint treatment. Parents will be instructed if the harness or splint can be removed for bathing and pampering or if the splint might be needed full time. The splints and braces will have to be adjusted time by time to the growth of the child.
In certain intervals follow up examinations have to be done, either with ultrasound, when the children are becoming older also with x rays.
Is it easy to treat a child with a hip dysplasia?
Generally the outcome of a therapy is much better the earlier the diagnosis is confirmed. The later a hip dysplasia is detected the longer a treatment might be needed. As an important part of the treatment is usually done as an outpatient treatment the patient compliance is an integral part of the treatment. Therefore the doctor will exactly explain the treatment steps and requirements to the parents.
What if my child need a surgery?
In severe cases surgical options might have to be discussed. The pediatric orthopedic surgeon will then explain the necessary steps of treatment detailed with the parents and the family.
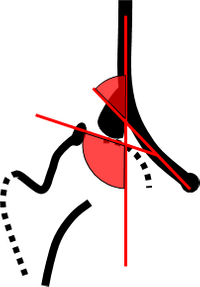
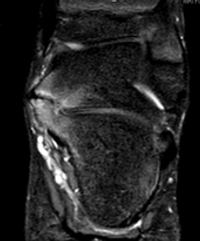
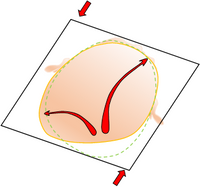
Example for an intraoperative setup
Which kind of surgical procedures might have to be done?
In case a treatment is not successful with conservative treatment or the hip situation is not allowing a stable reduction of the hip surgical options might be needed.
With closed or open reductions of the hips it is possible to relocate instable hips to a physiologic hip position. This position usually needs to be held stable with a special hip spica cast for a period of 6 weeks to 3 months to allow the joint to grow stable around the repositioned femoral head. During the casting period the child’s needs special hygiene care in which families are instructed. In case a cast needs to be applied for a period of 3 months a cast change after 6 weeks is done. These treatments will usually be done under general anesthesia during a short in-patient treatment at the hospital.
In cases where the bony acetabular roof is not developed properly from at an age from 15 months to 8 years a reconstruction of the acetabulum with an Acetabuloplasty is usually performed. Therefore a bone graft will be applied in the acetabulum bone to create sufficient acetabular coverage to protect the hip from dislocation. Sometimes in older children this needs to be combined with an adaption of the upper part of the femur bone to allow the femoral head to stay centered in the joint.
Before surgery: Bilateral hip dysplasia with dislocation on the left side
After surgery: bilateral Acetabuloplasty and open reconstruction on the left side
Several other techniques of hip reconstruction are published and can be performed related to the pathologic findings of the child. In case the treating pediatric orthopedic surgeon will discuss the treatment option in detail with the parents.
Is there any possibility to protect the hip of a newborn?
During the first month of life the baby’s hips have a normal flexion tone. This flexion tone should be initially protected. Extension of the hips with swaddling should be avoided. Specific baby slings and papoose are on the market, which support the knees of the baby and protect the baby’s hips during carrying time. Vitamin D3 Prophylaxis allows sufficient bone metabolism and reduces the probability of ossification delay.
How long is the follow up period in DDH after it is healed?
The follow up needs to be done until maturity. During the growth period there is always possibility for developing secondary dysplasia of the hips which should be ruled out during growth within certain intervals. Your treating pediatric orthopedic surgeon will guide you regarding these intervals. Usually these are done at the age of 3 years, 5-6years, in puberty and after end of growth.
TARSAL COALITIONES
The skeletal elements in the area of the distal extremity systems are already separated from each other in the 8th week of intrauterine fetal development. If this separation process in the area of joints remains incomplete, this consecutively leads to the formation of coalitions, which in many cases occur on both extremity sides, right and left. These coalitions are initially fibrous and somehow mobile, later cartilage-like and can continue to ossify to the formation of an incomplete or complete bony bridge. These fibrous, cartilaginous or bony bridges affect the usual free mobility of the tarsal bones which are functioning like a precise clockwork, thus causing foot pain due to overuse and sheer forces in the tarsal bones.
Coalitions are among the most common diseases of the child’s foot in need of surgical treatment. Their occurrence is indicated with a prevalence of about 1% (compared to idiopathic clubfoot 0.1-0.2%). However, many cases remain asymptomatic and are not diagnosed or diagnosed late.
It is not uncommon for real or supposed foot trauma to be the onset of clinical symptoms. In some cases spontaneous improvement of acute complaints is possible, so conservative treatment options are appropriate in some cases, while a surgical procedure must be considered for persistent complaints.
Calcaneonavicular Coalition
This is a very common form of the tarsal coalition. Usually in between the navicular and the calcaneal bone there is a ligament ( ligamentum bifurcatum). In a coalition this ligament is transformed into a fibrous, and at the age of about 8 to 12 years of life increasingly bony bridge. This causes reduced and inhibited tarsal mobility with limitation in particular of inversion and eversion which then often leads to stress pain. Also peroneal spasms and overuse pathologies in the Talonavicular joint are seen.
As a diagnosis apart from the restricted inversion and eversion mobility a simple X-ray usually shows already the problem. A MRI can confirm fibrous pathologies which sometimes can make diagnostic problems.
Therapeutically early resection, independent of the extent of the symptoms, is recommended. The prognosis is particularly favorable with early surgery.
Talocalcaneare Coalition
The second more important form of tarsal coalitions is found in the medial area of the ankle joint, most often involving the medial, middle facet of the talocalcaneal joint. The expansion of the initially fibrous, later increasingly ossified bridge formation can include very different parts of the lower ankle. Pain often occurs between the ages of about 12 to 16 years in the area of the coalition, but often also at the lateral side of the foot due to decreased mobility in the sinus-tarsi area as typical anterolateral subtalar impingement.
Besides the clinical symptoms of reduced mobility and pain the typical signs of talar head ossifications and C-sign in the X-ray can lead to the diagnosis. In these cases a MRI or CT scan is recommended to help the surgeon planning the treatment.
The indication of the surgical treatment is particularly difficult in the talocalcaneal coalition in childhood and adolescens. A resection here does not necessarily guarantee a painfree situation but an early treatment usually has a higher success rate after surgical treatment. There are some other important factors involved in the decision finding of the most successful treatment as e.g. muscular contracture status and presented foot deformities.
The postoperative follow up can be extremely lengthy with months of residual complaints. This is due to the fact that the joints have been in certain situations and alignments for many years and the resection of the coalition only creates the basis for the restoration of a certain partial mobility. In a certain percentage a secondary correction of the position of the foot or complete arthrodesis of the joint might be needed. Here especially in the talocalcaneal coalitions a secondary arthrodesis might in case be a reasonable solution for an otherwise secondary painfree situation.
The results of resection deteriorate with advancing age at the time of the procedure.
Tips for children’s foot health
On average, every person walks about 50,000 kilometers on foot in the course of his or her life. This distance corresponds approximately to a walk around the earth. In order to maintain the health of the foot for a lifetime, it is important to give the feet the necessary attention as early as in childhood. With regular foot care and attention the danger of permanent damage to the feet can be reduced effectively.
Dangers for the feet
The biggest dangers for the feet are inappropriate footwear, obesity and lack of exercise. If the conditions are unfavorable, then the development of the foot and gait pattern can be permanently disturbed. As a result, the muscles can shorten, the anatomy can change or the toe position can become worse.
How to find the right footwear
The main task of a children’s shoe is to protect them from external influences. The shoe should be comfortable, avoid injuries and protect from dirt and danger. The foot must not be restricted in its freedom of movement. The toes should have enough space and not be squeezes. The shoe must adapt to the movements of the foot and provide enough space for physiologic movement. The soles of the shoe need to be soft and flexible.
Regular barefoot walking as a prevention
The protective effect and the need for shoes is undisputed. However, it is necessary to walk barefoot regularly. Children exercise by barefoot walking and running all the foot related muscles. If muscles are not trained then the performance of gait might suffer. For this reason, parents should have their children walking barefoot on different surfaces for a defined period of time during the day.
Bow legs and Knock-knees can be normal
In the different stages of development, the leg position and the foot position change. The physiologic development of the axis of the legs changes from bowlegs to knock-knees during certain phases in childhood. Caution is advised when the children increasingly stumble over their own feet while running or if side differences are noticeable. At the age of 6 to 8 years the axes of the legs should be straight and symmetric. To clarify undesirable developments, a pediatric orthopedic doctor is the right person to contact.
Enormous growth in childhood
Children’s feet grow by up to three shoe sizes per year depending on their age and development. The growth is usually in spurts. It is normal that children have the same shoe size over several months and the foot then suddenly grows by one or two shoe sizes. In order to prevent surprises, parents should regularly, for example once a month, measure their children’s feet. When the shoes are worn every day, it is checked whether there is enough space between the tip of the big toe and the shoe. In this case, the shoe fits the toddler perfectly. The child’s foot should be checked on a daily basis to allow to find bruises, blisters, overuse symptoms, injuries or other unexpected developments.
Basic rules for the purchase and usage of children’s shoes
Children’s shoes are usually square or round shaped. Tight and too narrow shoes should be avoided for toddlers because the toes in this footwear do not get enough freedom. Anti-slip soles provide the necessary support, even in wet weather and on slippery surfaces. Rubber boots are water repellent and suitable for autumn days. Soft upper leather with a cuddly filling is the right choice on the winter walk. Socks with a high percentage of cotton support the beneficial effect of breathability of natural shoe materials in children shoes. On the other hand, when it comes to water-repellent Goretex shoes, a high proportion of synthetics is required. If shoes are moist after day usage and sweating enough time for drying during the night should be given. Daily change of used socks is important. The weight of the shoes should be rather light than heavy. The lighter the shoes are, the more the muscles are relieved. For the summer light footwear, such as sandals or sports shoes are ideal. Regularly check the inner sole and inside the shoe to avoid little stones, nails and other unpleasant foreign bodies to disturb your child’s gait pattern and comfort. High heels in children are generally not recommended as those are interfering with the foot stability, increasing injury risk and forefoot overload.
Several studies have found that almost every third child wears shoes that are too small. Unlike adolescents and adults, infants rarely express their discomfort in this regard. The sensitivity is reduced in the foot area, since the bones are still relatively deformable and the nervous system has to develop even further. The foot adapts to the shoe and wearing after a short time is no longer perceived as unpleasant. Only at the age of 14 to 16 the development of the feet is completed. The parents must therefore make sure that the shoe is suitable for the foot.
Pediatric Head deformities
Pediatric Head deformities
Pediatric head deformities are often seen as unnecessary to treat as they would anyway disappear spontaneously. What if not….
Why does a baby’s head become a deformity?
The skull of a baby is a very thin bone which grows within the first year tremendously. The volume of the head doubles within the first 6 to 7 months of life. Dependent on gravity and weight load, the skull bone is shaped and flattened in the weight bearing areas, as long as the child is mainly lying in its bed.
Some head deformities even developed before birth or even during birth. Those usually become better within a short period after the child is born.
Since the 1990 the incidence of head deformities is increasing, as the prophylaxis campaign of sudden infant death demands to position babies on the back while sleeping. Especially it the head is pointy consequently the head will tilt and rotate to one side.
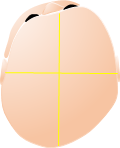
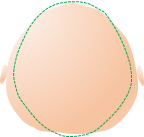
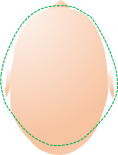
In case a child is positioning on one side preferably the skull flattens on this side and the exact opposite side which shapes a parallelogram like pattern of the whole skull. This pattern is called Plagiocephaly (“Plagio” Greek=oblique).
In case the baby would permanently be positioned on the back of the head a flat dorsal head could develop. This is called Brachycephaly (brachy= short).
Sometimes babies have orthopedic conditions which force the head to tilt in a certain position e.g. if one of the neck muscles is too short or injured during birth. Then this restricted movement does not allow the child to symmetrically move or position the head.
In rare cases the growth plates in the child’s skull are fused or partially fused which causes the head consequently to grow into an asymmetric shape.
Is an oblique head a problem for the baby?
It is often said that the obliquity is just a cosmetic problem which does not make any significant problems to the children. Recent studies are showing an interesting relationship in between the development of the child itself as well as the head shape.
The question is always why a child takes one specific position to develop a head deformity. A certain number of children develop a head deformity secondary as their development does not necessarily follow the physiologic milestones. In these cases the child has a developmental disadvantage and as a result the head shape changes due to the developmental delay, for example the inability to turn to one side, or the inability to free itself out of a certain position.
These children should be diagnosed properly and treated. Specific neurodevelopmental Physiotherapy can help these children developing their abilities. Very often then the head shape corrects within a reasonable timeframe.
Generally spoken we want to be as much symmetric as possible in the skull, as symmetry should be given in the eyes, ears, jaws, the basis of the cervical spine. Long term studies are still missing to scientifically confirm whether the oblique skull will really lead to increased numbers of orthodontic problems like crossbite or problems like migraine, cervical spine problems etc.
How can a pathologic head shape be diagnosed?
Your pediatrician or pediatric orthopedic doctor usually makes a complete examination of your child. Head shape, range of motion and development will be examined. Sometimes an ultrasound of the head helps to rule out more significant growth plate related deformities.
How can a plagiocephaly be avoided or treated?
There a different treatment options if you discover an obliquity of your child’s head. These are dependent on the individual age and development of the baby. Your pediatric orthopedic doctor or pediatrician can help you in the diagnosis and discuss with you the treatment options.
Positioning therapy, positioning of the bed in relation to room attractions and toys, alternate breastfeeding can help adapting the baby’s head rotation to both sides.
Daily “tummy time” under observation will strengthen the related neck muscles and decrease the load on the head and can prevent positional head deformities
There are certain either wedged or donut shaped pillows which can be placed under the mattress or the bedsheet to proper align the baby’s head. Here the actual guidelines to prevent sudden infant death do recommend a positioning therapy but do also explicitly restrict to put pillows in infant’s beds.
Specific developmental Physiotherapy (Bobath, Vojta) can help improving the baby’s milestone and motoric development.
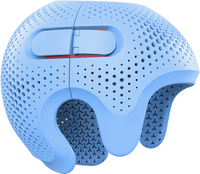
In case the deformity will not improve up to a certain age a helmet therapy can guide the growth of the head to a proper alignment over time.
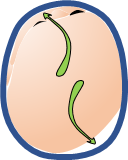
What does the helmet treatment do?
Individually measured and produced Helmets will guide the growth of the head without putting pressure to the physiologic growth. With the individual shape of these Helmets growth is distributed more in the areas which are more deficient in growth, so automatically the head shape corrects during further growth. The Helmet should be worn about 23 hours during a day in this time. In relation to any other therapy Helmets can correct Head deformities fast and safe
When is the best time to start a helmet treatment?
As the head grows significantly within the first year of life and the growth speed is less active after the first year it is an advantage to be finished with the helmet treatment at the age of about one year. To achieve an appropriate result your doctor might recommend the treatment depending on the clinical findings between the age of 6 to 8 months, to be finished with the treatment at the age of 1 year. A helmet treatment which is started too late might have to be continued for a longer period of time and might not be able to completely correct the head deformity.
Are there any risks or downsides involved in doing the helmet treatment?
Modern Helmets are ultra-lightweight, often 3D printed and extremely air ventilated, so that the possibility of sweating, skin irritation and pressure marks under the helmet can be minimized.
In case the insurance does not cover the cost there are expenses for the manufacturing of the helmet. These can vary dependent on the used materials and need for adaptions. Usually a specific maintenance of the helmet and usually digital head measurement follow up is included in the cost.
Summary:
The therapy of head deformities requires an early and stage related therapy which has a n excellent outcome if parents are involved and instructed. Prophylaxis of head deformities has a major impact on the development and is easy to do if instructed regularly. In case a deformity develops stage related therapy from adaption of daily habits, positioning, to physiotherapy and orthotic treatment with Helmets is a proven therapy pathway.
Dr. Michael Vohrer
Peadiatric Orthopaedic Surgeon
Circle Care Clinic
Plagiocephaly
mild
modreate
severe
Brachycephaly
asymmetric Brachycephaly
Plagiocephaly
Scaphocephaly
Plagiocephaly
Helmet function
Vitamen D
Vitamin D – Not only important for the bones…..
Vitamin D – one of the most important Vitamins for the human body – that important that the body produces it itself – if he has the chance for it. This means, if the body gets exposed to sun, vitamin D is produced, if the body is covered, protected with sun-screen or dressed with layers of clothing this cutaneous transformation and production of Vitamin D is inhibited.
Vitamin D is not only important for strong Bones and Muscle performance. A Deficiency is related to a couple of other Diseases like Dementia and Cancer.
No other Vitamin has a likewise high importance and function to the body. Well known is that Vitamin D protects our body from infections and increases our immune competence. Therefore it is important to get enough sun exposure, as this increases the endogenous production of Vitamin D in the body. Therefore Vitamin D is often known as “Sun Vitamin”.
Many people are not aware that Vitamin D is a variety of different Vitamins, D1 to D5, whereas the most important is Vit D3, Cholecalciferol. Several steps of synthesis are needed to transform it into the biologic active form.
As other Vitamins like B, C and E have to be taken by food, Vitamin D can be produced alone by the own body, provided that UV radiation from sunlight is exposed to the skin surface. Here on the surface of the skin Vit D precursor lipoproteins which contain Cholesterol are transformed in the biological active Vitamin D3. 80-90% of the Vitamin D demand is usually covered this way. This is at about 20 microgram per day. Accumulated excess of Vit D3 will be stored in the body for example in the liver and fat tissue. In low-sunlight season the body can consume these reserves out of its storage. The remaining 20% of Vitamin D demand will usually be supplemented with food rich in Vitamin D. Fat fish like herring and salmon, liver, mushrooms and egg yellow are rich on Vitamin D. Nevertheless a quite enormous amount of these nutrients would have to be consumed to get considerable amount of Vitamin D.
Vitamin D is a precursor for various hormons, constantly new functions are scientifically proven. Not only in the hormonal system and in the immune system Vit D has a key role. Meanwhile we know that almost any cell of the body carries a Vitamin D receptor. The action spectrum of this Vitamin could be even bigger than now already know.
Immune system:
Without Vitamin D some immune cells are not able to work. These T cells belong to the group of Lymphocytes. Vitamin D has an important double function. On the one hand it stimulates the production of defense cells, on the other hand it modulates the excessive immune defense to a standard. This is why Vitamin D is so important in autoimmune diseases like rheumatoid arthritis or even multiple sclerosis.
Bone metabolism:
Vitamin D is important to mineralize the bone. It regulates the mechanism of the bone building cells, the osteoclasts. Hence Vitamin D is that important for the bone as calcium. Most popular example for a deficiency in Vitamin D is rickets. Vitamin D Deficiency is still related with axial deformities and overuse problems in children and adults, like bow legs, knock knees, flatfeet and overuse pathologies like Osgood-Schlatter disease and Severs disease.
Muscle System:
Vitamin D supports muscle development and growth and protects to a certain extent against age related muscle loss.
Brain and nervous system:
Multiple studies have shown that Vitamin D has a preventive effect in relation to certain diseases of brain and nerves like Alzheimers disease, dementia, Parkinsons disease and even strokes. Additionally it is able to reduce the risk of falling in elderly people, a high risk factor for care dependency due to femoral neck fracture, confinement to bed and immobility.
Depression:
New studies are showing a relationship in between Depression and significant Vit D Deficiency. Also the so called winter depression caused by lack of sunlight can be treated with Vit D supplementation.
Cancer:
Fact is that in low-sunlight areas the cancer rate is higher than in regions closer to the equator. Reason for that can be that lack of sunlight causes Vit D Deficiency. Studies have shown that Vitamin D can reduce the proliferation rate of cancer cells. This seems to effective in bowel cancer, lung cancer and breast cancer. However, further studies in this field are ongoing.
Diabetes:
There are references that Vitamin D can effect the blood sugar positively. The Diabetes metabolism benefits significantly with Vitamin D.
Cardiovascular diseases:
Vitamin D could have protective effect on reducing vascular plaque development, therefore it would help prophylactically to reduce the risk for myocardial infarction and strokes.
Pregnancies:
During a pregnancy Vit D takes responsibility that the child is developing properly and that the mother is protected against gestational diabetes.
Sexual system:
The hormonal regulation is dependent in many ways from Vitamin, which is a hormonal precursor. Here Vitamin D supports the Production of sexual hormones. Good Vitamin D supply is linked to adequate Testosteron production in men and can improve fertility in men and women.
Vit D against overweight:
In a study with overweight children it has been shown that the body mass index BMI is reduced, that body fat reduces and that blood fat parameters improve as soon as children are supplemented with Vitamin D.
A majority of people, not only in Europe but also in sunny countries like the UAE are Vitamin D Deficient. As a reasons for a persistent Vitamin D deficiency in the population can be seen the use of Sunscreen products, which are for logical reasons used to prevent skin cancer and sunburns. The used UV block unfortunately also blocks the Vit D production in the skin.
Fine dust and smog are reducing the amount of sunbeams significantly which reflect on the skin.
Some people rarely go outside. Years ago these have been the elderly people and chronic sick patients. Nowadays the youth belongs to this risk-group as they rarely spend time outside in the fresh air and gardens.
Cultural clothing with covered appearance avoids direct UV exposure.
Signs of Vitamin D Deficiency:
The signs of Vitamin D Deficiency are unfortunately not always clear. Susceptibility for infection, bone pain, skeletal deformities, Tiredness and Depression are just a few examples pointing out to this problem.
Who wants to be sure can make a simple blood test which can diagnose the blood level objectively. Then a treatment program can be adjusted.
General recommendations are daily dosages of 400 units Vit D3 for children up to one year and about 1000 Units for older children.
An overdosage is hardly possible, as liver and kidneys need to transform the Vit D into its active form. This will only be done if there is really need and demand, otherwise it stays inactive.
With Vitamin D supplements a deficiency situation can easily be treated. A variety of Vit D3 products are on the market to make supplementation easy for each group of age.
The hormonal regulation is dependent in many ways from Vitamin, which is a hormonal precursor. Here Vitamin D supports the Production of sexual hormones. Good Vitamin D supply is linked to adequate Testosteron production in men and can improve fertility in men and women.
Vit D against overweight:
In a study with overweight children it has been shown that the body mass index BMI is reduced, that body fat reduces and that blood fat parameters improve as soon as children are supplemented with Vitamin D.
A majority of people, not only in Europe but also in sunny countries like the UAE are Vitamin D Deficient. As a reasons for a persistent Vitamin D deficiency in the population can be seen the use of Sunscreen products, which are for logical reasons used to prevent skin cancer and sunburns. The used UV block unfortunately also blocks the Vit D production in the skin.
Fine dust and smog are reducing the amount of sunbeams significantly which reflect on the skin.
Some people rarely go outside. Years ago these have been the elderly people and chronic sick patients. Nowadays the youth belongs to this risk-group as they rarely spend time outside in the fresh air and gardens.
Cultural clothing with covered appearance avoids direct UV exposure.
Signs of Vitamin D Deficiency:
The signs of Vitamin D Deficiency are unfortunately not always clear. Susceptibility for infection, bone pain, skeletal deformities, Tiredness and Depression are just a few examples pointing out to this problem.
Who wants to be sure can make a simple blood test which can diagnose the blood level objectively. Then a treatment program can be adjusted.
General recommendations are daily dosages of 400 units Vit D3 for children up to one year and about 1000 Units for older children.
An overdosage is hardly possible, as liver and kidneys need to transform the Vit D into its active form. This will only be done if there is really need and demand, otherwise it stays inactive.
With Vitamin D supplements a deficiency situation can easily be treated. A variety of Vit D3 products are on the market to make supplementation easy for each group of age.
Clubfoot And Its Treatment
Questions and Answers about Clubfoot and its treatment….
Club foot is common, affecting around 150,000 children worldwide every year – but it can be treated.
What is a club foot?
Club foot is a congenital abnormality of the foot with a combination of deformities like equinus and varus, adduction and cavus. There are lots of different types of club feet related to various medical problems. Club feet are also seen in neurologic or in some musculoskeletal disorders, e.g. cerebral palsy, spina bifida, arthrogryposis multiplex congenital and others.
Is it common among newborn in the UAE?
The most common club foot is the idiopathic club foot which has an incidence of about one to three per 1,000 births. More girls than boys are born with club feet and in about 25 to 50 percent of affected children the club feet are bilateral.
What is the reason for a clubfoot?
Genetic factors and environmental influences during pregnancy might play a role in the development of congenital club foot. There is not a single gene which is responsible for the development of club feet but several genes. Families with a history of club feet have a higher risk to have children with club feet, than families without any history.
The risk is particularly high if both the parents have club feet. These club feet are generally more severe than the sporadic idiopathic club feet.
Would a parent see it straight away?
Usually, most parents can see the deformity directly after birth as the feet are positioned inward, rotated and plantar flexed, and the mobility of the foot is restricted.
If parents are worried about the foot alignment after birth it is recommended to see a paediatric orthopaedic doctor to evaluate the deformity at the same time a general orthopaedic check-up can be done. Nurses and doctors are trained to see deformities and will guide the families to a paediatric orthopaedic doctor for evaluation.
Generally it is always recommended to do a hip screening (with ultrasound) at the age of four to six weeks to rule out other musculoskeletal problems like developmental dysplasia of the hip. In case of a clubfoot deformity this hip screening should be done before starting to treat the foot.
Can the clubfoot deformity be cured?
A club foot can be treated and cured by somebody who is experienced in musculoskeletal problems. The golden standard in club foot treatment is Ponseti Treatment. This method is a non-surgical treatment for correcting club foot. It involves three phases: four to eight weeks of weekly casting, a tenotomy (cutting of the Achilles tendon), which is performed in the clinic, and thereafter cast treatment followed by special shoes connected by a bar.
What is involved in curing it? Is the procedure painful for the baby?
The initial casting procedure is not at all painful for the child. After the initial castings the child undergoes a minor office procedure (tenotomy) done with local anaesthesia. Then a final cast is applied for three weeks. Thus, a baby who is treated from birth will have completed all casting by the age of three months.
When the last cast is removed after the tenotomy, the shoes and bar are applied. The child wears them day and night for four months. After the fourth month they switch to a “night time and nap time only” protocol and wear the shoes and bar only at night and nap time 14-16 hours per day until the age of four.
CONCLUSION: The Ponseti treatment is not painful and will be done with gentle manipulation by a specially trained pediatric orthopaedic surgeon. Usually outcomes in Ponseti clubfoot treatment are excellent if done properly by doctor and the affected family.














.jpg/picture-200?_=1768e801398)



.jpg/picture-200?_=1768eba5d78)

